Hip Procedure Grows Popular Despite Doubt (NYTimes)
It is one of the most popular operations in sports medicine. It comes in various forms, all with the same name: Hip impingement or bone shaving surgery. World-renowned athletes have had the operation — the Yankees’ third baseman Alex Rodriguez had it about two years ago and the sprinter Tyson Gay had it last summer.
But some sports medicine researchers are asking: where is the evidence that shaving bone helps? Might the bumps or irregular shapes they call impingement be just normal variations? Does the shaved bone grow back?
And it is not just professional athletes who are having the operation. Now some surgeons are even operating on teenage athletes with hip pain.
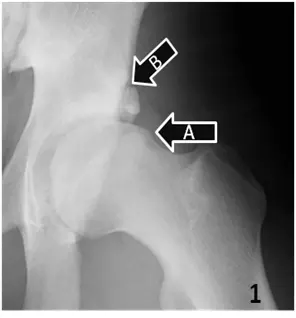
The idea is that bone that has rough edges or an irregular shape in the hip is rubbing against soft tissue in the joint, causing tendons to fray or muscles to tear. The hope is that by shaving and smoothing the bone, surgeons can protect patients from further injury and also protect them from developing arthritis. The amount of bone removed varies but can be significant — sometimes, as much as a third of the thigh bone’s top.
One difficulty in assessing the operation’s effects is that it is combined with other procedures to repair torn tissue. When patients say they feel better, is that because their impingement was fixed or because their torn tissue was repaired, or both? Another is that it takes years for arthritis to develop so it will take years for studies to determine if it has been prevented.
The combination surgery also complicates efforts to estimate the cost of the operations because it is billed under a variety of codes. The cost is also hard to evaluate because medical centers say that their charges are proprietary information. But at one academic medical center, the orthopedist’s charge for hip impingement surgery is about $4,400. The doctor’s charge to repair torn cartilage is an additional $4,400. Hospital charges are extra, as are charges for the months-long rehabilitation, but insurers almost always pay less than what is charged for the operation.
Yet despite the popularity of hip impingement surgery, said Dr. Harry E. Rubash of Harvard Medical School, “no one has really proven that it is uniformly helpful to the patient.”
Dr. Freddie H. Fu, chairman of orthopedic surgery at the University of Pittsburgh School of Medicine, said he had sought more evidence. “I challenge these people all the time,” he said. “I’m all for progress in medicine, but I want to do it right.”
Many surgeons are convinced the operation is necessary, even without high-quality evidence. Patients often have no idea there is a controversy and say the surgery took away what had been disabling pain. “I had no pain immediately after the surgery — none,” said Melissa Stephens, 37, of DeKalb, Ill. “It was like night and day.”
Surgeons who embrace the operation reason that bumps on the hip bones can eat away at cartilage, resulting, years later, in severe arthritis.
As evidence that the operation is helpful, they cite what are known as case series — descriptions of patients followed for relatively short times. But the problem with case series is that often doctors, without necessarily consciously doing so, may select patients who are likely to do well, with or without the procedure in question. And when patients are asked if they feel better after a major operation, many are inclined to say they do, often as a way of justifying such an onerous procedure.
Of course, the advocates of impingement surgery could be right. The problem is getting evidence to show it before putting more patients through a difficult operation.
One of the first to popularize impingement surgery was Dr. Marc J. Philippon, an orthopedic surgeon in Vail, Colo. He began doing it on athletes a decade ago. Then, he said, as orthopedists and athletes and patients with hip injuries started hearing about his results, there was more demand. Added to that, he said, were better ways of diagnosing impingement. In the past, Dr. Philippon said, impingement often went unrecognized and patients were told they had groin pulls — injuries common in runners and hockey and football players, whose sports involve repeated flexing of the hip.
Often the athletes tear their labrum, a rim of cartilage that surrounds and seals the hip joint. If the hip bone has bumps or is asymmetrical, orthopedists reason, those conditions may have caused the torn labrum and fixing the bone might prevent further injury.
“More and more orthopedists are doing it,” Dr. Philippon said. “It is part of the sports medicine armamentarium now.”
Dr. Philippon has operated on scores of athletes, many of whom, like Mr. Rodriguez and Mr. Gay, are famous. Mr. Rodriguez’s case is complicated. He returned to play but was questioned about whether he also took illegal performance enhancing drugs to help him do so. After his surgery. Mr. Rodriguez was treated by a Canadian doctor, Anthony Galea, who was indicted for giving performance enhancing drugs to athletes.
Dr. Galea said he treated Mr. Rodriguez only for “a damaged hip” that was “inflamed.” Dr. Philippon said that he knew nothing about that and that Mr. Rodriquez’s hip was fine after the surgery.
In his published papers — case series — Dr. Philippon reported that athletes’ hip injuries improved after the operation and that their hip pain remained at bay for at least two years. He said he would soon publish data following some professional athletes for 10 years.
But researchers say many questions remain. Among the most pressing is whether the procedure prevents arthritis.
One recent study cast doubt. Dr. George Hartofilakidis and his colleagues at the University of Athens in Greece followed 96 people with an average age of 49 with hip impingement but no hip pain. They did not have impingement surgery.
After 18 ½ years, 20 percent had developed arthritis, a rate that is not particularly unexpected as people age. There was no reason to blame impingement for it. So the researchers concluded that “prophylactic surgery is not warranted.”
Yet Dr. John J. Callaghan of the University of Iowa said his study indicated there can be a link to arthritis. The patients were in their 50s, did not have impingement surgery, and needed hip replacements because they had severe arthritis. Seventy percent had impingement. Nonetheless, Dr. Callaghan said, it is not known whether the bone shaving or reshaping operation can prevent arthritis or even whether the operation’s sometimes dramatic pain relieving effects last.
“We have absolutely no clue to whether the bone will grow back,” Dr. Callaghan said. “There are investigators who are working hard to follow patients, but unfortunately there are a lot of patients being operated on who are probably not being followed long term.”
This article has been revised to reflect the following correction:
Correction: November 16, 2011
An earlier version of this article gave an incorrect surname for a patient in DeKalb, Ill., who said bone-shaving surgery relieved her hip pain. She is Melissa Stephens, not Melissa Domb.