“Biologics Revolution > Breaking Down Barriers to Entry for Advanced Biologic Solutions” – A Guest Post by MedCap Advisors
About MedCap
MedCap’s team are specialists in medical technology, business strategy, and M&A. MedCap keeps a singular focus on developing growth strategies and implementing them through mergers, acquisitions, divestitures, and licensing agreements. As a result of their commitment to this industry, they have a unique global perspective on healthcare and deep understanding of the value of clinical efficacy, intellectual property, regulatory approval, reimbursement and, most importantly, unparalleled industry contacts.
—————-Beginning of the Article—————–
The steady growth of biologics in medical procedures is a signal that the industry is due for a significant change – the days of man-made materials ruling the drug and device industry are clearly numbered. Though the common perception is that biologics will not be prevalent for many years, the truth is that these advances are making an impact now and expansion is inevitable. We will continue to observe an increasing tension between philosophies of “repair” versus “regeneration.”
While man-made materials will always have a place in the case of acute trauma, biologics have the potential to take over all degenerative conditions. In the U.S., this may be accelerated by the recently upheld Affordable Healthcare Act, which eliminates insurance companies’ ability to exclude coverage for pre-existing conditions. This will lead to coverage for more patients for a higher class of medical solutions, including biologics.
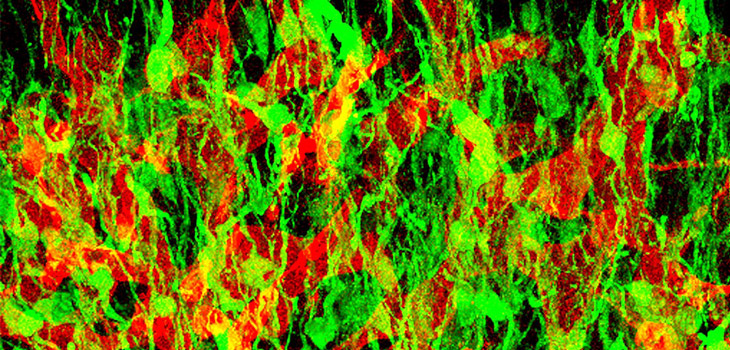
Biologics are already taking great strides, particularly in the field of orthopedics. Allograft tissue transplants, such as those offered by the Musculoskeletal Transplant Foundation (MTF) and Allosource in sports medicine treatments, are presently employed for ligament reconstruction, cartilage repair, and meniscal transplantation and spine fusion. Bone Morphogenetic Proteins (BMPs) are helping broken bones regenerate and heal. Synthetic bone graft substitutes are providing biologically active alternatives with the opportunity for greater global expansion due to reduced ethical, cultural and regulatory limitations. Implant surface modifications are improving implant integration, bone formation and wound healing. 3D printing of biocompatible materials is addressing the increasing need for transplantable tissues and organs. Fat transfers are literally transforming patients disfigured from disease and injury. Non-embryonic stem cells represent the next generation of medicine for everything from Parkinson’s to Alzheimer’s and, possibly in the future, organ tissue regeneration.
Using naturally occurring cells to treat diseases, fractures and other ailments is the ultimate goal of biologics pioneers. Progress can be seen in hospitals across the world, whether in the form of injecting Platelet Rich Plasma (PRP) into an injured Major League Baseball player’s arm or using stem cells to treat and heal a patient recovering from necrotizing fasciitis (flesh-eating bacteria).[1] This growth is forcing the surrounding markets to evolve or fade away as biologics continue to mature.
The metal implant arena serves as a prime example, as issues with deteriorating devices have led to waning confidence in traditional technology. The Associated Press reported that “metal hips accounted for about 27 percent of all hip implants in 2010, down from nearly 40 percent in 2008. Doctors have begun turning away from the implants amid several high-profile recalls, including J&J’s recall of 93,000 metal hips in 2010.”[2] Due to increased concerns over the “leak of traces of metals into the bloodstream,” the UK’s 2012 Medicines and Healthcare products Regulatory Agency (MHRA) guidelines suggested “annual check-ups should be continued for the life of the implant” for patients with “metal-on-metal” hip implants, instead of the earlier recommended five years post-surgical annual check-ups.[3]
The immediate solution may be to return to ceramic and plastic coating; in the long term, biologics will play a prominent role in improving implant procedures. However, the advancement of biological materials, implants, and technologies still faces hurdles that must be overcome before the market can fully develop.
Barriers to Biologics
As the science of biologics grows, the market and regulators are struggling to keep pace. Residing in a gray area between pharmaceuticals and traditional technology, biologics face several roadblocks to widespread adoption: integrating with the medical device industry, clarifying Food and Drug Administration (FDA) regulations, manufacturing and product quality, and updating patent guidelines are high priorities for advocates.
Medical device industry must give ground
The medical device industry is a natural opponent to biologics entrants, and the sheer size and power of the companies in play ensure a healthy resistance. The device industry – including world class organizations like Johnson & Johnson, Biomet, and Zimmer – stands to lose significant market share for metal or synthetic implants, especially in the orthopedics arena. To the extent that biologics succeed medically and financially, they will replace or diminish the need for the current style of implants.
Biologics pose a threat on a number of fronts. The extraordinary ability to heal body parts through bioreactive agents rather than replacing them with a synthetic facsimile presents seemingly limitless potential in medicine. Biologics are also predicted to be less expensive than metal implants, and they promise higher and longer lasting success rates in patients.
Eventually, corporations that have been positioned as opponents or observers will join the biologics revolution. Market pressures will steer them to acquire biologics to get the most lucrative product into their pipelines; they will look to complement their traditional portfolio of medical devices with newer, stronger products.
FDA is still finding its footing
The strength of medical device giants unfortunately introduces a controversial factor in the FDA’s approach to biologics. Major companies have the resources and motivation to exert influence over the FDA’s approach to regulating biologics; certainly slowing approval is in their best interests.
Their activity hampers development by small companies and deters investment by venture capitalists, cramping the FDA’s responsibility to protect patients and ensure that the advancement of science and patient care is not derailed by corporate interests. This influence is best evidenced by the fact that many safe and efficacious biologic treatments to degenerative disease are available in developed countries and less developed countries around the globe. In these countries, the reimbursement for conventional implants is not nearly as high as the reimbursement in the US, and corporate interests do not have as much at stake.
Further clouding the issue, market regulation for biological products under the FDA often navigates through overlapping laws and unexplored science. With biologics still a nascent discipline, the FDA has trouble evaluating products that typically have no precedent in the system. This often results in lengthy research processes, adding delays to the market launch of biological innovations. Further data collected in human patients from around the world is not often accepted by the FDA, thereby forcing costly and time consuming studies.
Part of the difficulty in overseeing biologics can be traced to the initial administrative attempts to categorize them. The FDA’s drug sector was home to biological studies until the Center for Biologics Evaluation and Research (CBER) was created in 1987. Starting in 2002, the FDA began categorizing certain biologics as “drugs”, hoping to achieve swifter reviews from the Center for Drug Evaluation and Research (CDER).[4] However, as the CDER was structured primarily to evaluate chemicals in pharmaceuticals, the introduction of cell research has been a more painstaking effort than anticipated.
Despite these setbacks, the U.S. is making inroads to nurture the burgeoning field. The Biologics Price Competition and Innovation Act of 2009 offers a shorter approval pathway for biological products that are similar to an FDA-approved item. The BPCI Act aligns with the FDA’s longstanding policy of accepting what is already known about a drug, therefore saving time and resources and avoiding unnecessary testing that would further delay the progress of new biologics products.[5]
The FDA attempts to provide an added layer of defense against intellectual property theft through the data exclusivity stipulations outlined in the BPCI and supplemented in the Reference Product Exclusivity for Biological Products File Under Section 351(a) of the Public Health Service Act. While the FDA has recently attempted to clarify the process needed to guarantee 12-year exclusivity, approval eligibility can vary depending on the version of the biologic in question and other numerous exceptions.[6] Furthermore, negotiations for the 12 country Trans-Pacific Partnership (TPP) free trade agreement (including the US) have placed in contention this 12 year exclusivity period in favor of a possible 7 year period, shortening data protection for biologics by 5 years.[7]
Patents struggle with the burden of proof
In the same way that the FDA has difficulty defining biologics for the sake of regulation, the patent system seems at a loss as to how to introduce them into its system.
Traditional pharma products are composed of chemicals that can be evaluated for bioequivalence of intellectual property in a strict linear formula. The same cannot be said for biologics, which are built on cells with immense complexity, including variations in phenotyping and amino acid sequencing. To compensate, the patent office studies products for biosimilarity, a categorization more difficult to prove in a conventional sense as it must take into account the multitude of variants between cells, the majority of which do not compare directly. The arduous research process unfortunately makes for weaker cases for developers seeking to gain patent protection by proving the similarity to (or difference from) a competitor’s source cell.
The number of patent filings for all drugs has been falling, but the drop in small molecule patents has been more precipitous. In 2009 biologics accounted for 60% of all drug patent filings.
The uncertainty of the patent landscape has led to a “wild west” mentality. Developers are hesitant to share the secrets of their techniques, as the young industry leaves ample opportunity for competitors to stake claim to a previously unreported product or its process. With the parameters poorly defined, sometimes staying off-patent has proven the best way to avoid intellectual property theft.
Of course the industry will have to solidify protections before products can flourish. And urgency is growing, as a collection of patented biologics are scheduled to expire and make way for generic incarnations. With the process so unrefined, it will hinder the emergence of generic, less expensive biologics – and lower cost delivery which is the key to faster adoption.
Volume is the most viable means to upgrading the biologics patenting system – here, practice makes perfect. Each year sees a growing collection of manufacturers taking the leap to patent their products to then submit for FDA approval. In the process, they are also giving the patent sector the opportunity to perfect its evaluation techniques. The FDA’s class of 2012 for approved biologics includes the likes of Clinimmune Labs and its HPC Cord Blood, a cell therapy indicated for use in hematopoietic and immunologic reconstitution.[8]
Biological materials that regenerate in the human body, as opposed to mimicking it, will lead humans to living better lives. Indeed, the use of metal and synthetic implants have exposed patients to high levels of toxic metals that leak their way into bloodstreams, muscles, and bones.[9] Biologics represent a safer, more cost-effective, and more advanced answer for patients and practitioners.
Leaders will need to emerge in the biologics marketplace to challenge the market barriers, paving the way for the sector to truly thrive. Researchers and developers must fight for recognition of their products as medically, legally, and financially legitimate, while buyers and physicians must have the right channels to put them into practice.
Bone regeneration and healing treatments have progressed from the limitedly available autograft bone grafts, to the at times contentious bone morphogenic protein, to highly bioactive and reliable synthetic bone graft substitutes.
[1] Young, Biloine W. “Osiris Stem Cells Treat Flesh-Eating Bacteria.”
Orthopedics This Week. June 2012.
[2] Perrone, Matthew, “FDA panel sees little use for metal on metal hips”. Boston Globe, June 28, 2012.
[3] http://www.nhs.uk/Conditions/Hip-replacement/Pages/Metal-on-metalimplants.aspx
[4] Reid, Ken. “CBER and CDER have long history of being lumped together and split up.”
Bioresearch Monitoring Alert Sept. 2002.
[5] Assessing the Impact of a Safe and Equitable Biosimilar Policy in the United States, May 2, 2007.
http://www.gpo.gov/fdsys/pkg/CHRG-110hhrg40500/html/CHRG-110hhrg40500.htm
[6] FDA.gov, 2012 Biological License Application Approvals.
http://www.fda.gov/BiologicsBloodVaccines/DevelopmentApprovalProcess/BiologicalApprovalsbyYear/ucm289008.htm
[7] http://www.biopharma-reporter.com/Markets-Regulations/US-FDA-tweaks-requirements-for-12-year-biologics-exclusivity
[8] http://www.biopharminternational.com/patent-exclusivity-biologics-seven-or-twelve-years?rel=canonical
[9] Rattue, Grace. “Metal Hip Implant Concerns – Potentially Bigger Scandal Than Brest Implants.”
Medical News Today. February 2012.

 The Orthopedics Industry
The Orthopedics Industry