
This is the fourteenth in a series of 6-Question interviews with leaders who are challenging conventional thinking in Orthopedics (read other interviews here).
I believe that VR Surgical Training and Surgical Planning will become the norm in Orthopedics over the next decade. As this technology continues to demonstrate its value, we will one day look back and wonder why surgeons ever learned on live patients in the OR and practiced on cadavers in labs.
As with all new technologies in orthopedics, there are always first movers. VR Training is no exception.
I sat with Dr Danny Goel to better understand how Precision OS is leading this training revolution in orthopedics.
1) Why is orthopedic surgical education perfect now for virtual reality?
The current mode of teaching surgery has its roots in apprenticeship, where students learn under the tutelage of an experienced master. Around the turn of the 20th century, elements of formalized education were introduced, but since then, nothing else has really changed. In the meantime, we’ve seen all this innovation with new surgical devices, new implants and new procedures. So, there’s a lot more to learn. After their five years of residency training, new surgeons haven’t always received the training they need to be fully autonomous or ready for independent practice.
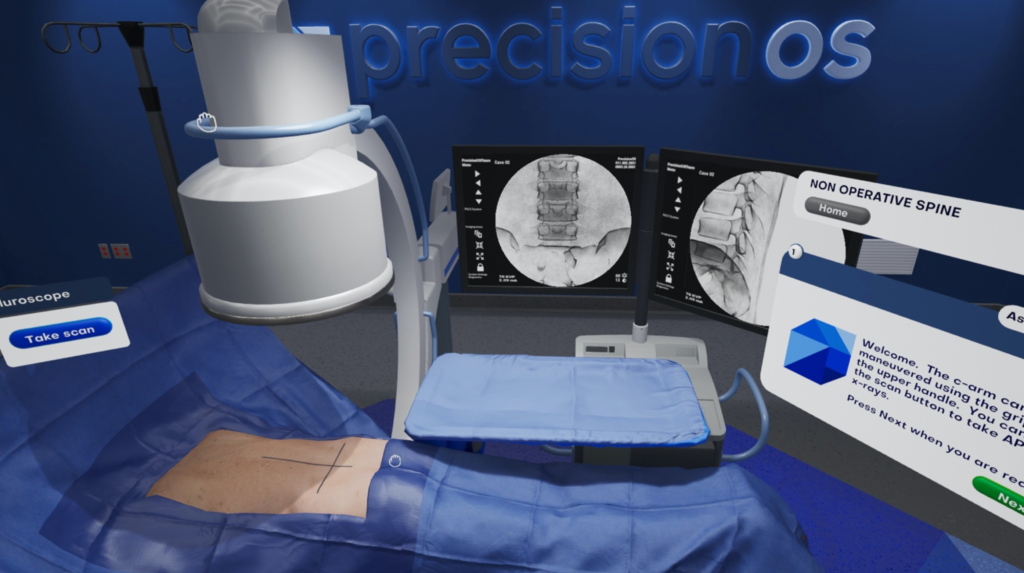
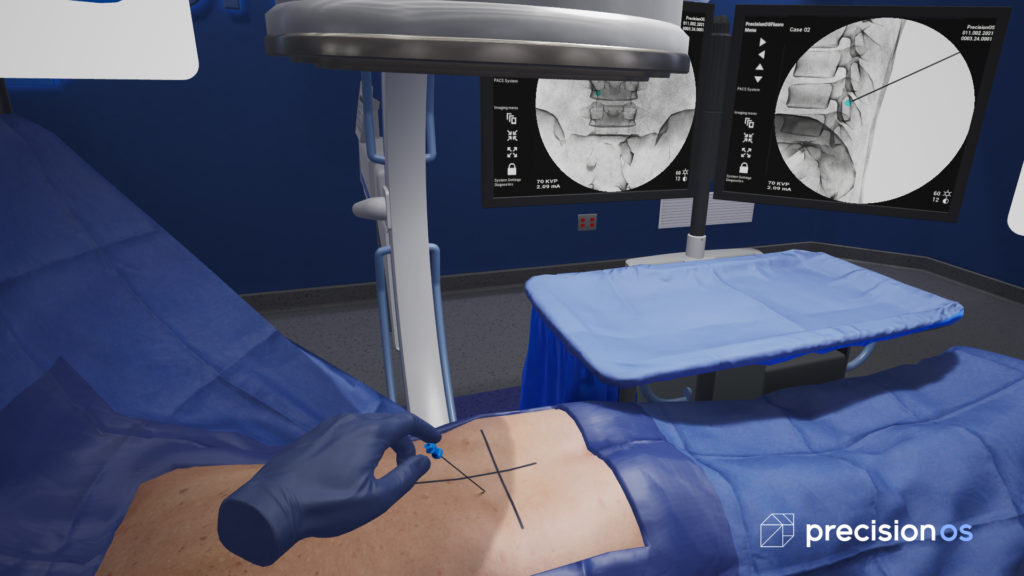
At the same time, virtual reality has advanced to the point where the software, hardware and artistry have come together to allow us to create extremely realistic, high-fidelity experiences. That gives us the opportunity to change how surgery is taught. We can make the learning more personalized, rather than time-based. We can provide a safe medium for people to make mistakes, using a principle known as productive failure, which obviously isn’t possible with a living patient. Another principle that hasn’t been talked about much is voluntary instability. This is the idea of pushing yourself to a point that is uncomfortable, but without the overhanging stress that impacts performance. This opportunity doesn’t really exist during live surgery. It’s already a stressful environment and performing sub optimally in this environment has its obvious challenges.
We can also introduce the variability that you see in real life. There’s a misconception in surgery that if you do 200 joints, you will be an expert. That’s not completely true. Ask any surgeon and they will agree that every case presents something unique. You become an expert by experiencing the variability that individual cases represent. With virtual reality you can practice multiple times, with multiple variations, over and over again and receive real-time feedback on performance. Allowing users to improve their skills and ability to think and react swiftly in a real-world OR—that’s how you become an expert.
2) How did Precision OS get started? What was the light bulb moment?
I met Rob, our Chief Creative Officer, through our kids. I was telling Rob about an idea I had for an app that would educate family physicians about how to triage orthopedic-related cases. I have always been interested in physician access and findings solutions that allow patients to receive efficient and accurate health care without waiting. Rob said, “Well, you should really look at VR and meet Colin because he’s doing some work in that area right now.” When Colin, now our Chief Technical Officer, showed me the virtual headset and I put it on, that was the epiphany. The experience was totally different, realistic and extremely impressive. Shortly after that, we got together to seriously discuss the business idea that eventually became Precision OS.
3) What are the advantages and disadvantages of a medical device startup based in Canada?
The perceived disadvantage of being in Canada is that we don’t carry the weight and investor pool that comes with being in the Bay Area/Silicon Valley. Having said that, there are several, perhaps unknown, highlights of being in Vancouver that have started to attract our neighbors from the south. Vancouver has a rich history of game development, artistry and visual effects. Furthermore, the VRAR ecosystem is flourishing, as there is a large concentration of impressive VR companies in Vancouver. The local VRAR association has done an incredible job promoting and showcasing globally what we and others are doing, which has helped Vancouver become the second largest VRAR hub in the world. That, in addition to hosting many major orthopedic meetings, makes it a great area for medical device start-ups to get exposure. Overall, I feel very fortunate that we started our company here.
4) There are other VR surgery training startups. What is your secret sauce at Precision OS?
This is a great question and is really one you have to experience. We do get many comments from people who say they didn’t know what VR could actually do or accomplish until they experienced what we have created. A lot of this stems from the fact that we are thinking beyond the current pedagogical approach and augmenting ways to provide surgical education. The foundation of our company has been to remain patient centered. With this in mind, every team member understands that our decisions are made in the interest of providing the most in-depth, focused and quality education we can deliver. This has led to some very interesting group discussions.
For example, we once debated for over an hour about how people put a puzzle together. It sounds trivial but the discussion lead to a solution for our product. This abstraction and depth is what you will see in all aspects of our content from the look, feel and data you are provided. We are then combining both the cognitive and technical aspect of surgery into one experience. This has had considerable impact on our industry partners, and in a manner they have not seen before. Others are recreating what we do in cadavers and sawbones and bringing that into virtual reality. We are not thinking that way. We are challenging the current method of education and don’t want to recreate what we currently do. We’re focused on changing the paradigm, adding significant layers of depth and value to our customers and to peoples’ learning. There is a massive shift happening in surgical education for both the industry and for surgeons like myself. Our team is focused on the content the technology can deliver and the problem that it’s solving. Also, as a university-affiliated surgeon, understanding and talking with my colleagues using this technology, we have approached VR using a very academic, evidenced-based approach. We completed a multi-center randomized blinded controlled trial with the Canadian Shoulder and Elbow Society in 2019. Senior residents were randomized and received either virtual reality or traditional learning. Then they were assessed by unbiased surgeons from across Canada, using a validated outcome score while performing surgery on cadavers. Notable findings include increased technical proficiency among those who had the VR training. The most striking finding was the VR group demonstrated and 570% greater efficiency in learning. This means you could learn in minutes using Precision OS compared to traditional methods.
We also get asked commonly why the focus on realism. It’s a long answer but the short version is this: We are in the healthcare space and assisting those dealing with patients. I know when I’m teaching a course, in the OR to a resident, the greatest memory that most people will have is when they experienced something real. We have designed our realism and the accuracy of our technology to be authentic. Physicians need to care in virtual reality in order for them to care in real life. By delivering a high level of psychological and physical fidelity, it makes users feel they are part of a real OR environment. Combining that with the ability to fail is a completely different experience that keeps physicians empathetic and creates a more active and effective surgical learning experience. That’s a really important training element for us and drives the data we are collecting. It is also the major and noted difference between us and our competitors. But don’t take our word for it, we’ve had numerous reviews of surgeons all over North America who have provided testimonials on our website.
5) What is the current product, and what is the regulatory pathway in the US?
I would say we have two products. One is on the education side, and it’s being used by surgeons and residency programs as well as by medical device companies to educate their sales reps. That requires no regulatory pathway because it’s an educational tool.

The second one is our preoperative planning tool, for surgeons in practice. This will allow surgeons to plan and execute in the virtual world and make small but important adjustments to their approach to help optimize the case outcome. That is currently going through the FDA regulatory process and we hope to launch in mid-2020.
6) Where is the future of VR and AR in surgery going?
This is perhaps one of the most exciting parts for all of us at Precision OS. We’re going to be able to create and train physicians all over the world in a way that minimizes the disparity in health care. We can see a future where every patient will have access to physicians with similar, advanced training and expertise. We’ll be able to utilize experts in different parts of the world to support physicians anywhere in the world and truly deliver value-based care—the right patient, treated by the right surgeon at the right time—on a global scale. That’s a big vision by itself. But VR will also allow for further innovation in ways we can’t even comprehend, because we’re just starting to tap into the potential that VR and AR offers. We feel that VR and AR will change not only the way we train and educate but also perform cases while having profound research implications. Most importantly, they will have a significant impact on quality of life and outcomes for patients around the globe.
You can learn more about Precision OS at:
Website: https://www.precisionostech.com/
Email: info@precisionostech.com
Phone: 877-673-0176
Address: 321 Water Street, Suite 500
Vancouver BC Canada V6B 1B8

 The Orthopedics Industry
The Orthopedics Industry