 Restoring Cartilage: The Holy Grail of Orthopaedics (JBJS Case Connections)
Restoring Cartilage: The Holy Grail of Orthopaedics (JBJS Case Connections)
Introduction
Theoretically, articular cartilage restoration should be a solvable biological/mechanical problem. But repairing, restoring, or replacing hyaline cartilage and the matrix that supports it presents formidable physiological and physical challenges. For decades, researchers have been investigating many different methods of cartilage repair, and no approach has yet risen to “gold standard” status.
As the “Current Concepts Review” in the February 19, 2014, edition of JBJS points out, the main strategy for cartilage “self-repair” is bone marrow stimulation, primarily via microfracture. Restorative/replacement approaches focus on cartilaginous constructs composed of allogenic, autogenic, or tissue-engineered materials.
This month’s “Case Connections” looks at four cases involving three different restorative/replacement approaches to cartilage defects. The variable outcomes emphasize the gaps between theoretical and clinical solutions to this common skeletal problem.
Is “Young” Allograft Better?
In the June 24, 2015, edition of JBJS Case Connector, Ramirez et al. report on a high-school quarterback whose full-thickness glenoid osteochondral defect was filled arthroscopically with particulated juvenile cartilage allograft. The sixteen-year-old football player presented with a two-month history of right shoulder pain and a feeling of instability, precipitated by a tackle during a football game.
Physical exam revealed forward shoulder elevation to 150° with moderate pain but no muscle atrophy. External rotation was 60°, and the shoulder rotated internally to the T7 vertebral level with pain and crepitus. Anterior apprehension, relocation, and load-shift tests were all positive.
Radiographs showed a 2 × 2-cm lucency in the inferior-central region of the glenoid. MRI showed an anterior-inferior labral tear and an osteochondral glenoid defect that measured 1.7 × 2.5 cm. After a period of unsuccessful nonoperative management, diagnostic arthroscopy revealed a displaced anterior-inferior labrum and a full-thickness, 1.5 × 1.5-cm cartilage defect of the inferior-central region of the glenoid.
Surgeons repaired the labrum arthroscopically and then dried the surface of the defect by draining the arthroscopic fluid. A layer of fibrin glue was placed in the defect, followed by placement of particulated cartilage “chips” with an arthroscopic grasper and curets (Fig. 1). Surgeons smoothed the interface between the native glenoid cartilage and the graft and applied another layer of fibrin glue to secure the graft.
Arthroscopic image showing placement of particulated cartilage graft into an osteochondral lesion of the glenoid.
One week after surgery, the patient had smooth passive range of shoulder motion with minimal pain. Aided by a standard Bankart-repair rehab program, by six weeks he had no shoulder pain with activities of daily living, and at twelve weeks the shoulder exhibited 160° of elevation, 45° of external rotation, and internal rotation to T10. The patient began a supervised throwing program six months after surgery, at which time MRI demonstrated interval filling of the glenoid defect. He was participating fully in high school football nine months after surgery, with full, pain-free range of shoulder motion and strength. These positive outcomes persisted at the most recent (two-year) follow-up.
The authors emphasized that the particulated cartilage used in this patient was obtained from a donor younger than thirteen years of age. Such “young” allograft tissue presumably contains “better” chondrocytes than those from an older donor.
How Long-Lived Are Allograft Chondrocytes?
As Ramirez et al. implied, the variable quality of allograft cartilage is a concern for orthopaedic surgeons. Surgeons aren’t sure whether samples from tissue banks come from donors with marginal-quality cartilage to begin with, or whether the tissue has been stored in ways that optimize chondrocyte viability. To address the question of cartilage-cell survival, Convery et al. analyzed the histological, cellular, and biochemical characteristics of an osteochondral allograft that had been in situ for ten years.
The allograft recipient was a twenty-eight-year-old male letter carrier who had injured his left knee playing baseball. Arthroscopic debridement had revealed a large defect of cartilage and bone in the left medial femoral condyle, and the patient eventually received a fresh osteochondral allograft that included approximately 6 mm of subchondral bone. During the next eight years, the patient experienced progressively worsening knee pain when walking and postambulatory aching. A second fresh cartilage allograft was implanted ten years after the first procedure. Intraoperatively, the initial allograft was found to be collapsed and split transversely, and surgeons carefully excised and analyzed a portion of it.
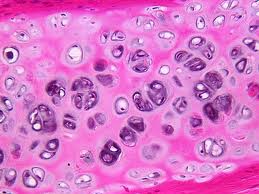
Histologically, the articular surface of the retrieved allograft was intact, and the chondrocytes appeared viable. Staining with safranin O-fast green confirmed the presence of glycosaminoglycans, further suggesting normal chondrocyte function. However, the remaining allograft bone was acellular and nonviable, suggesting that the in situ fracture and collapse were the result of bone resorption or failed incorporation. Using high-performance liquid chromatography, physicians determined the percentage of type-II collagen in the retrieved tissue to be >90%, further suggesting viable chondrocytes. However, the host cartilage surrounding the allograft contained only 60% type-II collagen.
Convery et al. concluded that “the [initial] graft in our patient did not fail as a result of metabolic activity of the articular cartilage but rather as a result of resorption of the transplanted subchondral allograft bone.” Consequently, these authors recommended placing additional autogenous bone beneath allografts to augment the host bed, thereby possibly enhancing incorporation of the osseous shell of the allograft.
Preventing Graft Hypertrophy
The challenges of recreating cartilage matrix were emphasized in a case report by Welsch et al. A forty-nine-year-old man with a trauma-related cartilage defect of the medial femoral condyle received a matrix-associated autologous chondrocyte transplant (MACT). Surgeons harvested and cultured the patient’s chondrocytes and seeded them into an implantable synthetic hyaluronan-based scaffold. MACT is thought to curtail the risk of graft hypertrophy in autologous chondrocyte transplants, partly by obviating the need for a periosteal flap.
Three months after the procedure, MRI revealed good repair fill and integration with adjacent cartilage. However, the patient experienced progressively reduced range of knee motion from four to twelve months after surgery, and MRI at twelve months revealed some hypertrophy of the repair tissue and more pronounced thickening of the medial tibial condyle in the area contacting the implant.
Deducing that tibial cartilage hypertrophy was the probable cause of declining knee function, surgeons recommended arthroscopy. Prior to the procedure, they evaluated the area with high-resolution biochemical MRI, which revealed reduced glycosaminoglycan content in both the femoral repair tissue and the hypertrophic tibial cartilage. Arthroscopy confirmed hypertrophic tibial cartilage, and histological analysis of resected hypertrophic tissue showed a mixture of fibrocartilage and hyaline cartilage. The range of knee motion improved markedly after arthroscopy, and the patient returned to work two weeks after the operation.
The authors speculated that a small part of the original MACT structure dislocated from the femoral condyle and attached to the articulating tibial condyle, where it matured into a hypertrophic state. The authors encouraged surgeons to consider hypertrophy of cartilage opposite a defect if range of motion and clinical symptoms occur after MACT.
Tissue-Engineered Cartilage: A Long Way to Go
Finally, Adachi et al. reported on the case of a thirty-six-year-old woman in whom corticosteroid-related osteonecrosis of the lateral and medial femoral condyles was treated with tissue-engineered cartilage combined with a hydroxyapatite scaffold enhanced with mesenchymal stem cells.
MRI and diagnostic arthroscopy confirmed a 25 × 20-mm osteonecrotic lesion on the medial femoral condyle and a slightly smaller lesion on the lateral condyle. Surgeons harvested and cultured 300 mg of cartilage from unloaded areas of the ipsilateral femoral condyles and bone marrow from the iliac crest.
As shown in Figure 2, surgeons removed necrotic bone from the medial condyle and made three osseous sockets in the center of the lesion. They placed cylindrical blocks of the hydroxyapatite into the sockets, injected them with stem cells cultured from the patient’s marrow, and sprayed fibrin glue onto the surface to prevent stem-cell leakage. Next, surgeons placed the tissue-engineered cartilage in the defect and sutured a synovial flap harvested from the patient’s suprapatellar pouch over the construct. Surgeons treated the lateral condyle with two hydroxyapatite blocks only.
Fig. 2-A Removal of detached cartilage and sclerotic subchondral bone from the medial femoral condyle. Fig. 2-BImplantation of hydroxyapatite blocks and cultured mesenchymal stem cells. Fig. 2-C Placement of tissue-engineered cartilage onto the lesion. Fig. 2-D Coverage of the construct with an autogenous synovial flap.
The patient reported that pain and clicking in the knee disappeared soon after the operation. Evaluative arthroscopy one year after surgery showed that the medial femoral lesion was covered with smooth cartilage-like tissue, and no osseous defects were apparent. Analysis of a biopsy sample from the medial femoral condyle showed a mixture of fibrous and cartilage-like tissue. Exposing the sample to safranin-O resulted in weaker staining than is seen with normal cartilage, suggesting a deficiency in proteoglycans in the regenerated tissue. Despite these mediocre histological/biochemical results, two years after implantation, MRI showed smooth and congruous tissue covering the medial condyle, and the patient was very satisfied with the results.
Although this patient had a good short-term clinical outcome, the authors cautioned that longer-term follow up “will be particularly important because histological examination of the biopsy specimen showed that the regenerated tissue was not true hyaline cartilage.”
Conclusion
These cases emphasize the many hurdles to successfully restoring cartilage, including growth of hyaline cartilage, mimicking the complex nature of the cartilage matrix, and incorporating the cartilage and matrix into the host subchondral bone.
The extent to which MRI and histological findings actually predict long-term clinical efficacy is unclear, and the variable natural history of untreated cartilage defects suggests that prospective studies with suitable control groups will be needed to prove the efficacy of restorative techniques. Nevertheless, early intervention with biologic restoration of the articular surface will eventually have a profound influence on patients with cartilage damage—and on the physicians who treat them.

 Tiger Buford – retained recruiter dissecting orthopedics
Tiger Buford – retained recruiter dissecting orthopedics 
