
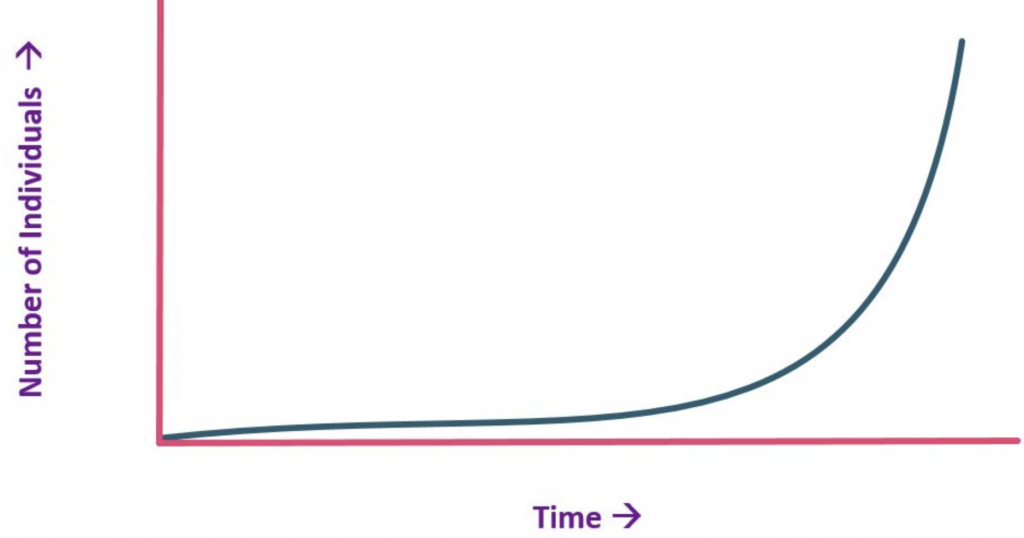
Mako Surgical was a great startup with exponential growth. Just look at these numbers that Mako produced before the 2013 Stryker acquisition.
- 2006 – first-in-man
- 2008 – 500 surgeries
- 2009 – 1,000 surgeries
- 2012 – 23,000 surgeries with a run rate of $100M gross sales
Message: If you want a high valuation for your orthopedic startup, you need to generate an exponential adoption rate.
Mako Surgical was founded and began by Rony Abovitz, Maurice Ferre M.D, and other members of Z-KAT, Inc. team in 2004. Together, they were developing a novel haptic robotic system for medical applications, such as their Whole Arm Manipulator which was originally developed at MIT and then at Barrett Technology.
Leading them to their creations of the Mako Robotic Arm. Martin Roche M.D performed the first MAKOplasty Partial Knee Replacement Procedure in 2006. Their company hit giant milestones within the first few years, performing 500 MAKOplasty procedures in 2008, 1000 by 2009, and more than 23,000 by 2012.
Mako SmartRobotics is a robotic-arm assisted surgery machine that uses three principal elements to perfect the process of total knee, total hip, and partial knee replacements to create better outcomes for patients in need. The three elements that are used in Mako SmartRobotics robotic-arm assisted surgery are AccuStop haptic technology, 3D CT-based planning, and the use of insightful data analytics.
Mako has become one of the most highly trusted surgery methods. Here are some of the accolades:
- More than 14+ years of robotic-arm assisted surgery experience with Mako SmartRobotics.
- More than 145+ published, peer-reviewed articles and studies have been published about the surgery system.
- Across 26 countries and every state in the contiguous United States, over 850+ systems have been installed and have been used for this practice.
- Over 1,000+ United States and foreign patents and patent applications have been established.
- Over 300k+ Mako procedures have been performed.
These are the awards that Mako has received:
- R&D Robotic 3D Visualization Surgical Tool Award for their RIO Robotic Arm Interactive Orthopedic System by Research and Development Magazine in 2010.
- Gold Medical Design Excellence Award in 2010.
- The Fast Tech Award for being one of the fastest-growing technology companies in South Florida by the South Florida Business Journal in 2010.
- No.1 on the Technology Fast 500 as the fastest growing technology company by Deloitte in 2011.
- Fast Tech Award as one of the 25 fastest-growing technology companies in South Florida by South Florida Business Journal in 2011.
- CSSEC Award for loyal, customer-focused staff members presented by the Technology Services Industry Association in 2011.
- ACE Award (Achievement in Customer Excellence) from MarketTools in 2011.
- South Florida Manufacturer of the Year by the South Florida Manufacturers Association in 2012.
But how does Mako robotic knee surgery work? Total Knee Replacement is done by removing the arthritic knee bone and cartilage and replacing it with an implant to reduce pain and restore the motion and functionality of the knee and leg.
In Mako Total Knee Replacement Surgery, the surgeon has to begin with a full CT scan of the knee joint which is done by taking a series of X-rays taken at different angles that can assist surgeons to see things they wouldn’t be able to with a standard X-Ray procedure. This data from the CT scan is then used to generate the 3D model of the patient’s anatomy.
The pre-operative plan is created from this model, by loading it into the Mako system’s software. This plan is also revised and looked over by the surgeon to ensure everything is correct and ready to go. In surgery, the surgeon locates points on the patient’s knee to load them into the Mako system, just as the 3D model was used for planning and in comparison to the joints on the 3D model.
Once the anatomy is registered to the 3D model, the surgeon can modify the plan, if desired. The surgeon uses the robotic arm as a tool, guiding it to remove the arthritic bone and cartilage on the knee. After this is done, the surgeon inserts the implant into the joint of the knee. The surgeon will check on the movement allowed by the implant and if it is up to their expectations, the patient can begin their recovery.
- In 2019 in the Journal of Arthroplasty, it was reported that there were less damage and fewer bone and periarticular soft tissue injuries in robot-assisted replacements.
- In a study from 2019 that was reported in the Surgical Technology International journal, it was discovered that patients who had used Mako technology were less likely to develop patella baja, which is a condition that affects the patella, overall flexion, and joint range of motion in the leg. This condition is more common in other methods of replacement.
- From another study in 2018 in the Journal of Knee Surgery, it was discovered that Mako cuts were closer and more precise based on original pre-operative plans than manual knee replacement surgery cuts.
- Within recovery, it was found that reduced total morphine consumption and a reduced length of hospital stay in a 2019 study presented at Orthopaedic Treatment Center.
- A greater improvement in functional activity such as walking and standing with higher scores at both 4-6 weeks and 6 months follow-up. This information was presented at the Knee Society Meeting in 2018.
- In a 2017 study in the Journal of Knee Surgery, it was reported that patients had an overall higher patient satisfaction scores.
- It was found that cost was less for those who used Mako technologies, due to less time having to stay in the hospital, decreased readmissions or doctor visits, and quicker recovery.

Mako total knee replacement is also known because it is said to Cut Less. It was found in a study that Mako surgeries had less bone and soft tissue damage in total knee replacement, reduced post-operative pain in partial knee replacements, and greater preservation and upkeep of bone stock in total hip replacements.
This is because Mako AccuStop haptic technology is used to guide and make the exact cuts planned, making sure they are precise, and this sometimes means that soft tissue or a healthy bone can be saved in the process.
Partial Knee Replacement depends on the severity and location of arthritis in the knee bone area, which will be the beginning of deciding if Mako is right for you. The lateral compartment, the medial compartment, and the patellofemoral compartment (also known as the kneecap) are the three sections of the knee. Total knee replacement is best and often the most recommended for when all three areas of the knee are affected and diseased.
When only one or two compartments are, that’s when partial knee replacement comes into play and may be recommended by your doctor. In this type of surgery, a surgeon only removes and replaces what is necessary, which helps the surrounding areas (the ligaments and bones).
Mako Partial Knee Replacement Surgery is done by removing the arthritic knee bone and cartilage and replacing it with an implant to reduce pain and to restore the motion and function of the knee. In Mako Partial Knee Replacement Surgery, the surgeon begins with a CT scan of the knee joint, exactly as if they were going to perform total knee surgery.
The rest of the process is almost exactly the same, or very similar to that of a total knee replacement. This CT uses your unique anatomy to form a 3D model. The pre-operative plan is created from this model, by loading it into the Mako system’s software. This plan is also revised and looked over by the surgeon to ensure everything is correct and ready to go.
In surgery, the surgeon locates points on the patient’s knee to load them into the Mako system, just as the 3D model was used for planning and in comparison to the joints on the 3D model. Once the anatomy is registered to the 3D model, the surgeon can modify the plan another time, looking for any issues or mistakes that could have been made along the way.
The surgeon uses the robotic arm as a tool, guiding it to remove the arthritic bone and cartilage on the knee. After this is done, the surgeon inserts the implant into the joint of the knee. The surgeon will check on the movement allowed by the implant and if it is up to their expectations, the patient can begin their recovery.
- From a study presented at The Partial Knee Meeting in Bruges, Belgium in 2018, it was found that Mako Partial Knee survivorship at 3-year follow-up was 99.2% for medial Unicompartmental arthroplasty and 100% for lateral Unicompartmental arthroplasty.
- In a 2016 study in the Journal of Bone and Joint Surgery, component position accuracy was found to be improved in patients who used Mako technologies compared to those who didn’t.
- Mako surgery led to a shorter time to straight leg raises, decreased number of PT sessions, reduced post-op pain, improved max knee flexion at discharge, and reduced mean time to hospital discharge was reported in a 2018 Bone Joint Journal study.
- No implant failure or implant-related complication or revision surgery, as well as excellent overall patient satisfaction for 96.1% of patients, was found in a 2019 European Journal of Orthopaedic Surgery & Traumatology study.
- In a 2018 J Arthroplasty study, overall outcomes at 2-years were better than patients who received manual surgeries.
It was found that overall cost after the surgery was overall for those who used Mako technologies due to less time having to stay in the hospital, decreased readmissions or doctor visits, and quicker recovery.
All surgeries are done by the surgeon guiding the robotic arm to remove arthritic bone and cartilage. This is very unique because the surgeon can also use a virtual boundary during the operation, along with other visual cues. Mako is a tool, not a surgeon. It is very important to recognize that tools like Mako change the game when it comes to knee replacement, but you will still need a trustable and notable surgeon who is specifically trained in the Mako system.
Only a dozen or so surgeons in Arizona are trained in Mako, so it is important to do your research to find one like Dr. Brian Gruber, MD, board certified orthopedic surgeon of Integrated Orthopedics who are specifically trained in using the Mako system.
Mako replacement surgery is intended for patients who have severe pain or stiffness resulting from noninflammatory degenerative joint diseases such as osteoarthritis, traumatic arthritis, or avascular necrosis, rheumatoid arthritis, or post-traumatic arthritis. Mako is also a good option for those who haven’t benefited from other options like bracing, medication, or joint fluid supplements and are ready to find their next step.
Mako is not intended for patients with specific infections, or for those who suffer from a mental or neuromuscular disorder that would create an unacceptable risk, those with prosthesis fixation failure because it would not work correctly, those who have experienced complications in postoperative care in the past, patients that have compromised bone stock in their body, people with skeletal immaturity, those with a severe instability of the joint in the leg, or excessive body weight.
Integrated Orthopedics offers total knee replacement surgery through Brian Gruber, MD, MBA, Board Certified Orthopedic Surgeon. Dr. Gruber is specifically trained in using the Mako system for Mako robotic knee surgery. He will discuss all options with a patient and so they can rest assured that he will lead them on the correct path.
It is important that you talk to a specialist before making your choice to use Mako SmartRobotics for your surgery. Schedule a consultation with Dr. Gruber today.

 Tiger Buford – retained recruiter dissecting orthopedics for you
Tiger Buford – retained recruiter dissecting orthopedics for you