(written by Bill Hunter, MD, President & CEO, Canary Medical for OrthoStreams)
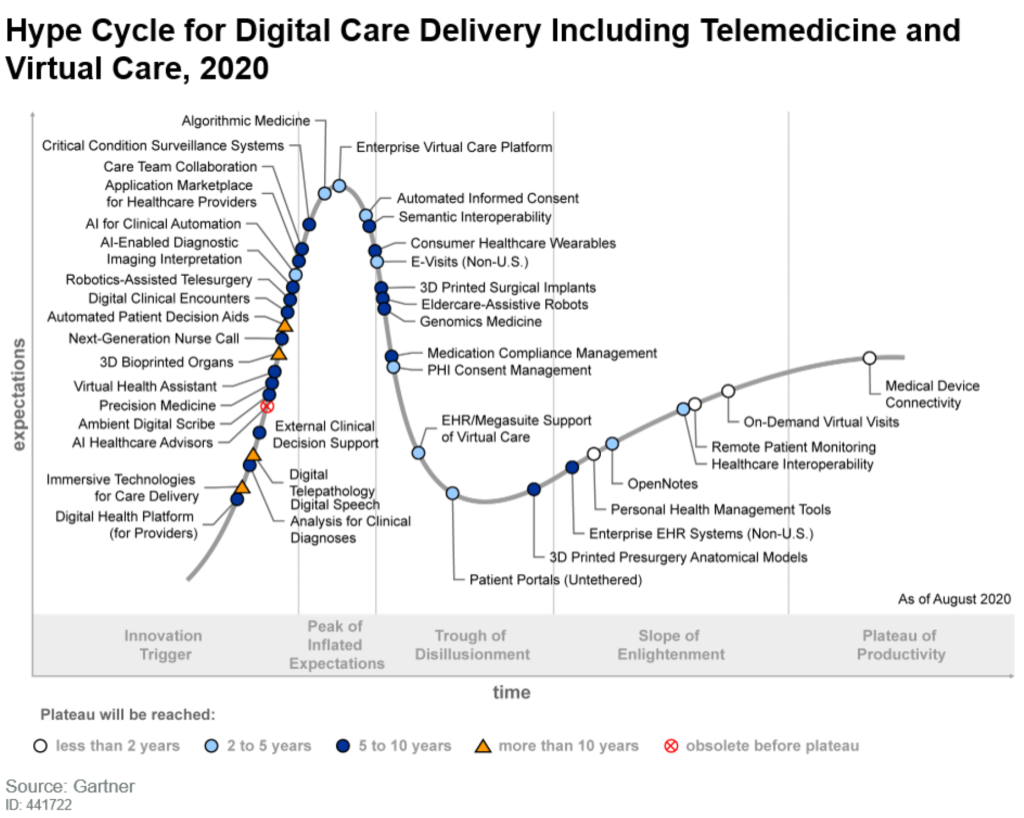
After a little over a decade of participating in the field of digital health, I have reached the conclusion that successful companies follow a predictable pathway based upon the growing number of patients they have under management:
Digital health companies begin as patient monitoring companies, become diagnostic companies, and evolve into patient management companies.
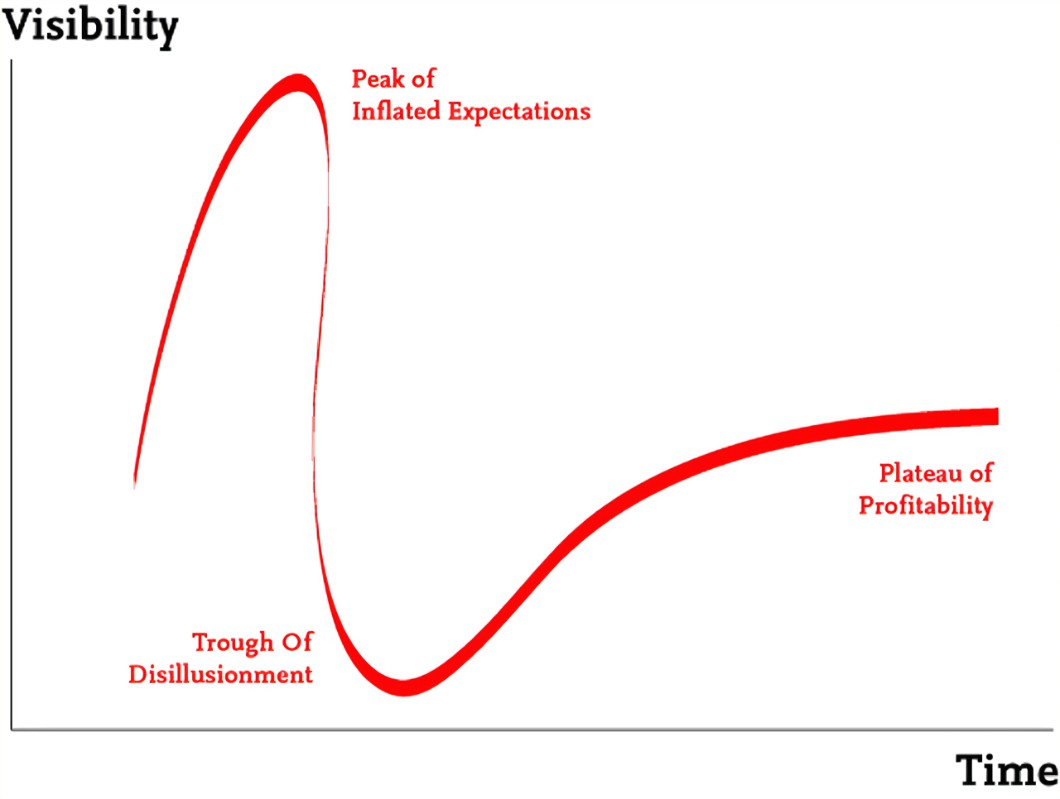
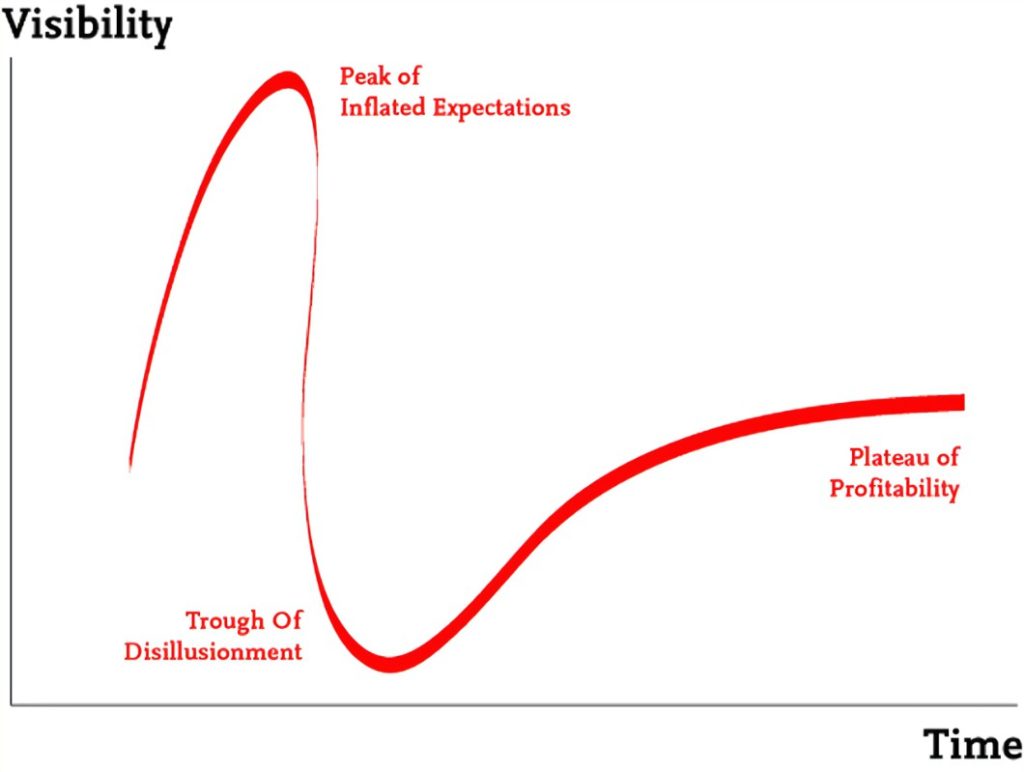
The Hype Cycle curve for digital care delivery is progressing along the pathway described below in Gartner (S. Hakkennes, L. Craft, M. Jones, 2020). As we enter the “Trough of Disillusionment” – at least with respect to investor sentiment and valuations – it is fair to ask, where this is all heading? Is digital care delivery a fad or a game changer? In situations like this, my colleague Michael Raynor has trained me to ask, “What job will the new technology perform?” and “Will the new technology make that job better, faster, more efficient, cheaper, or easier?” If it doesn’t perform an important job (a job that needs doing) and do that job at least 2 or 3 ways better than however the job is currently being done, it’s probably a fad.
To have a lasting impact, digital medicine must supplement traditional medicine (not the other way around!), so what are the jobs of practicing medicine and delivering patient care? Can digital health execute certain aspects of patient management better, faster, easier, and cheaper than the current standard of care? Since Tiger focuses on the orthopedic industry, I will use a product we are involved with, Persona IQ, as a specific example – but these principles can be applied to other products, specialties, and industries.
Job One: (Remote) Patient Monitoring
Regardless of specialty, all patient care begins with routine surveillance of the healthy patient. Regular checkups, “standard” blood tests and diagnostic imaging are utilized to make sure all is well, and importantly, quickly identify when things aren’t. Studies examining a plethora of clinical conditions have proven the medical and economic benefits of promoting disease prevention over disease treatment. Therefore, the first potential job of a product like Persona IQ is to perform routine patient monitoring more easily and efficiently by doing it remotely. The current job of patient surveillance has a few of drawbacks: it requires patient compliance (you have to show up for regular screening), it is episodic (any given test/exam is a “snapshot” in time, not a continuous readout), it is expensive (in both time and cost), consumes resources (physicians, technicians, equipment) needed for other purposes, and it is relatively inefficient (large populations must be screened to identify a small number of positive findings). Internal sensor placement has unique advantages: it has high patient compliance (almost 100%; versus 25-35% for wearables and 50% for clinical follow-up visits); data collection is continuous (daily versus episodic); the readings have high fidelity (collected inside the joint versus externally); it is cheaper than diagnostic imaging (serial x-rays, MRI); and it is collected autonomously (so it doesn’t increase clinical workload). It takes a few hundred patients and a few months of monitoring to observe/understand what “normal” and what “falling behind” look like, but identifying good/bad recovery patterns is a potentially valuable job to be done. Flagging struggling patients can target them for increased activity programs and enhanced physiotherapy, while reinforcing the “normal” recovery path of the rest can reduce anxiety and help set reasonable expectations. Therefore, a company’s first digital health product is one that can remotely monitor patients better, faster, more efficiently, more reliably, and cheaper.
Job Two: (Early) Diagnosis
The job of surveillance ends and the job of administering treatment begins once a diagnosis is made. I can think of very few (no?) pathological conditions where early diagnosis isn’t beneficial in terms of limiting severity, reducing treatment invasiveness, improving outcomes, and lowering costs. Unfortunately, in many cases, suboptimal surveillance has resulted in a patient presenting with an already well-established clinical condition. A costly workup of blood chemistry, imaging, diagnostic studies, and specialist consultation establishes the nature and magnitude of the problem at hand. A second important job for a “smart” implant is identifying “at risk” patients as quickly and efficiently as possible. After monitoring several thousand patients (10,000?) over a suitable time period, data sets can be collected from large cohorts of patients who recovered normally and from those who experienced complications. With sufficient examples of each, the normal/abnormal data sets can be compared using machine learning to uncover “differences” in the collected data patterns. Ultimately, the detected differences are used as “indicators” in future (naive) patients to estimate their relative risk (probability) of developing a specific clinical problem. It is the computer equivalent of a clinician looking at an ECG tracing to detect ischemia or myocarditis; it may not be 100% conclusive, but it provides clues as to what to look for. A TKA infection “diagnosed” (predicted) a few days in advance of a fulminant clinical presentation could be the difference between conservative management and a contaminated implant needing staged replacement. By collecting a large data set per patient (1 million data points in year one), it could be possible for Persona IQ to identify even subtle differences between normal and pathological recovery patterns. While the TKA story remains to be told, this approach is already being used by companies in asthma, COPD, diabetes, mental health, and hundreds of other conditions to create Digital Diagnostic Companies capable of identifying vulnerable patients. It is important to keep in mind the oft-used computer science adage of “garbage in, garbage out” – predictive accuracy depends on large patient numbers, clean data sets, and high quality “training” data (precise patient demographics, diagnostic results, detailed clinical progress notes, and accurate outcome measurements).
Job Three: Personalized Patient Management (to Improve Patient Outcomes)
Even superb diagnostic skills are wasted if the job of administering the right treatment, to the right patient, at the right time, is handled poorly. At the end of the day, this is where the vast majority of cost – human, economic, and HCP burnout – resides in healthcare. Once large, high quality data sets from tens of thousands of patients become available, it is possible for a digital health company to transform itself into a Digital Therapeutics Company. Large data sets collected the same way, from the same patients, using the same device, but from different centers with different practice patterns can yield a wealth of valuable population insights. What treatment regimens yield the best results? Which patient demographic benefits most from which type of treatment? The list of potential questions to be addressed is almost infinite. Personalized care has been the goal of medicine for decades now, and while digital health alone won’t provide the answer, it has the potential to be a very valuable tool. Digital insights are only as valuable as the treatment programs implemented to respond to them; an early diagnosis without a corresponding early and appropriate intervention is worthless. Pioneers in this field, companies like Teledoc, Livongo and Hinge, employ clinical staff (physicians, nurses, physiotherapists) to monitor patients, identify negative trends, respond to alerts, and administer the appropriate therapy on a patient-by-patient business. The ultimate goal is both simple and elusive: use a patient’s own data to deliver personalized care and improve clinical outcomes, reduce complications, and drive down costs. A thriving digital health company will likely find itself evolving into this business model for the simple reason that the true promise of their technology can never be unlocked without it.
Job Four: Go Back to Job One
If you are fortunate enough that everything has gone according to plan, you have a happy, healthy, high-functioning patient. You can now revert back to monitoring her remotely…until her other knee needs replacement.
written by :
Bill Hunter, MD
President & CEO, Canary Medical

 Tiger Buford – retained recruiter dissecting orthopedics
Tiger Buford – retained recruiter dissecting orthopedics